Peer Instruction in Medical Education
Peer instruction is an active learning technique designed to identify learning needs through problem solving and formative feedback. This supports deeper understanding of complex content and encourages higher-order thinking.
Peer instruction also helps address deficiencies in conceptual understanding that occur as a result of passive learning experiences. Peer instruction allows students to be more actively engaged in their learning, as it supports self-assessment to determine if concepts are understood.
During peer instruction, students work with their peers in small groups within a larger classroom environment. This involves providing students a few minutes to read and answer a question on their own, followed by another few minutes to discuss their answers in a small group, with the goal of coming to consensus on the correct answer. The instructor then leads a discussion regarding the correct answer, often asking students to volunteer to clarify and describe their rationale. Following this discussion, the instructor then provides feedback and elaborates on the correct answer and the student explanation. Peer instruction has become increasingly popular across multiple academic disciplines, including medical education.
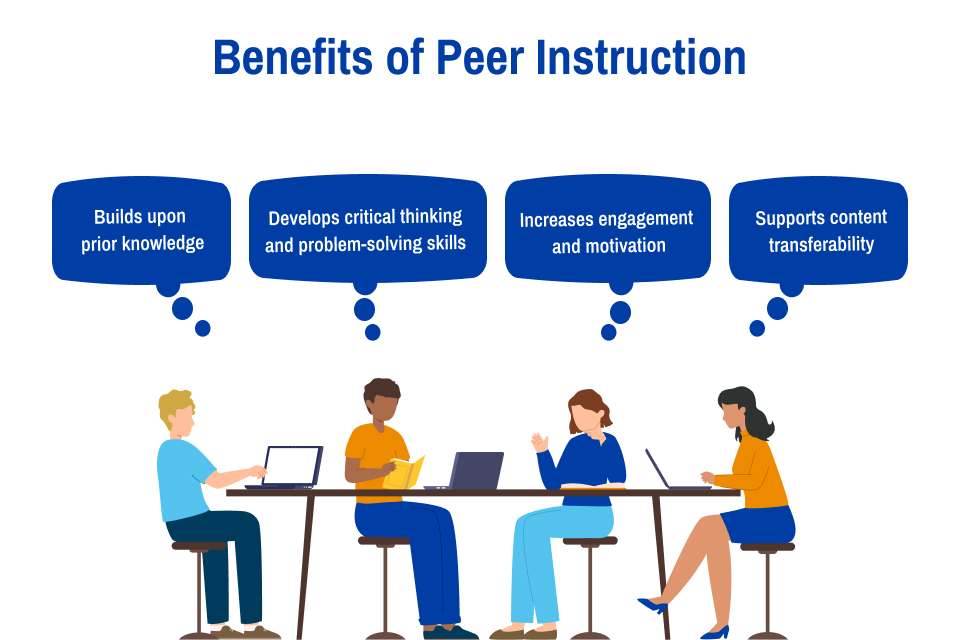
Benefits of Peer Instruction
Peer instruction in medical education allows adult learners to build upon prior knowledge, promoting a deeper understanding of complex medical and physiological concepts and relationships. Additionally, peer instruction allows students to further develop critical thinking and problem-solving skills, which can lead to better future patient outcomes. Peer instruction also increases engagement and motivation for learning, as immediate feedback is provided throughout the learning process. Overall, peer instruction promotes an active learning approach that allows medical students to learn, engage, collaborate, and develop communication skills relevant to their current and future training.
The scholarly literature offers evidence that peer instruction facilitates student comprehension and enhances meaningful learning. In a comparison study between peer instruction groups and nonpeer instruction groups, peer instruction increased student performance on multiple choice quiz questions by 27%. As an active learning technique, peer instruction can support lower performing learners in bringing their scores closer to their peers. Peer instruction is also valuable for content transferability. This means learned material can be extended from one context into many new contexts, which is effective for improving comprehension of complex medical topics. The practice and immediate feedback involved in peer instruction allows for this transfer of knowledge into new contexts. Further studies indicate that peer instruction can improve in-class problem-solving skills and ability to integrate material. This active learning encourages students to engage in their learning, think critically, and develop a deeper understanding of medical concepts.
Planning Peer Instruction
As you plan a peer instruction session, focus on student comprehension and long-term retention. To be effective, take the following into consideration:
- Develop learning objectives for the session and share them with students.
- Identify and curate pre-session resources aligned with the learning objectives for students to review prior to in-session time.
- Write questions that require deep conceptual thinking and understanding, have one correct answer, and align with the learning objectives.
- Use different types of questions measuring recall, conceptual understanding, relationships between concepts, or clinical knowledge depending on the topic and level of the students.
- Request feedback from mentors and peers who can review and offer feedback about question readability, appropriate distractors, and clinical relevance.
- Use an audience-response system that requires students to commit to an answer on their own and then defend that answer to their peers before agreeing on a final answer.
- During student explanations, probe for the ‘why’ and allow students the opportunity to explain their answer, defend their rationale, and explore relationships between concepts.
- Use data from the polls and other sources of feedback, such as conversations with students to evaluate the completed session, identifying strong points and areas of improvement to help guide future sessions.
At the Saint Louis University School of Medicine, peer instruction sessions are used to evaluate understanding of material after self-directed study. Students are presented with a question and have 90 seconds to submit an answer on their own. After, in small groups, students discuss and defend their answers for another 90 seconds before coming to a consensus and submitting answers again. Following this second discussion, a student is called on at random to explain their answer aloud to the entire class, while the professor probes for further information and asks follow-up questions. Peer instruction provides students with immediate formative feedback and an opportunity to collaborate with peers in the understanding of complex medical concepts. Moreover, active learning through problem solving and higher-order thinking supports learners in their ability to identify linkages between concepts and apply their new knowledge in future learning.
In summary, peer instruction promotes learning at multiple levels. In comparison to traditional lectures, peer instruction has overwhelmingly shown improvements in exam performance, understanding of material, and students’ ability to solve conceptual problems. Using peer instruction has the ability to make a profound impact on student learning and long-term retention.
 Abbey Haas is a medical student (Class of 2027) at Saint Louis University School of
Medicine. Abbey’s areas of professional interest include peer tutoring, pediatrics,
and oncology research. Abbey can be found on LinkedIn or contacted via email.
Abbey Haas is a medical student (Class of 2027) at Saint Louis University School of
Medicine. Abbey’s areas of professional interest include peer tutoring, pediatrics,
and oncology research. Abbey can be found on LinkedIn or contacted via email.